Fast PACE Start-Up and Expansion Guide
Background
Programs for the All-inclusive Care for the Elderly (PACE) provide health and social services to frail, older adults. PACE provides care to ~60,000 Americans, the vast majority of whom are dual Medicaid/Medicare eligible. With nearly 7.6 million Medicare-eligible and 2.2 million dual-eligible Americans living with complex needs, a significant opportunity exists to expand the number of PACE organizations (POs) to reach more seriously ill older adults. However, opening a new PACE site, or starting a new PACE organization, is a complex, expensive, and time-consuming process with factors such as staffing, financial planning, legal and regulatory considerations, location selection, building design, participant recruitment, and program development all needing to be addressed.
Online resources exist for some of these areas, but resources are not always easy to find, easy to cross-reference and some simply have not existed, making the process even more difficult. To address this, West Health developed a comprehensive resource hub for those looking to start or expand a PACE organization. The website (and downloadable guidebook) compiles, organizes, and directs users to existing resources and fills in gaps where resources did not previously exist. Attendees will be walked through this resource to support those who plan to start or expand a PO.
The National PACE Association’s (NPA) PACE 2.0 Initiative is leading the charge to accelerate PACE growth by improving access to PACE services for the eligible population. The PACE 2.0 Initiative Fact Sheet provides more information about the opportunity for PACE expansion.
Using the Fast PACE Start-Up and Expansion Guide
This resource is intended for those interested in starting a new Program of All-Inclusive Care for the Elderly (PACE) or looking to expand their existing PACE organization. It outlines the various topic areas that need to be considered when creating a successful program and provides linkage to existing resources. Please also refer to this step-by-step checklist, which organizes all content into actionable steps.
The goal of PACE is to allow nursing-home eligible individuals to remain independent and live in the community. To be PACE-eligible, individuals must be 55 years or older, certified to need nursing home-level care, live in a PACE service area, and be able to reside safely in the community with PACE support at the time of enrollment.
PACE is unique in that it is more expansive than a standard senior day center and provides more services and care than a traditional clinical practice.
For more information:
• National PACE Association’s Understanding PACE
• Centers for Medicare & Medicaid Services (CMS) PACE website
PACE Responsibilities
PACE organizations are responsible for all elements of clinical and social care, including:
- Primary care, physical and occupational therapy, nutrition, behavioral health, medication management, durable medical equipment, medication, testing and imaging
- Social work (including assessment and management of emotional and behavioral problems, coordination with family members and other support systems, connections and referrals to external/community-based social services and resources, etc.);
- Specialty care (specifically via coordination and referrals to external providers);
- Home care (including personal care, grooming, and money management);
- And, recreational therapy and social activities, via the physical day center where meals and opportunities for social support are provided.
For a current list of required services, visit Medicaid PACE Benefits.
In addition to the services that are required of all PACE organizations, there are many other optional programs that are frequently incorporated depending on participant need, staff interest and available resources, and availability of local partners for support. Below, a few examples of clinical and non-clinical programs often featured as part of PACE organizations are listed. Please note that this is not an exhaustive list of services covered by PACE.
- Palliative Care / Goals of Care
- End of Life Care and Bereavement
- Pain Management
- Behavioral Health
- Telehealth
- Caregiver Support
As of 2021, one third of the eligible PACE population is being served by a PACE organization.
This coverage gap implies an opportunity to open additional PACE centers, and those wishing to do so should complete NPA’s Organizational and Market Self-Assessment in advance. This assessment will provide valuable information about the demand for services in the relevant population and community, while assessing the sponsoring organization’s capacity to carry out services.
Analyze the results of the assessment with a consultant or Technical Assistance Center (TAC) before moving forward with the process. There is more information about consultants and TACs in the Engage Stakeholders section. The organizational and market assessment will help with choosing a service area. A service area is a group of zip codes that the new PACE center will service. Review the process for applying for a service area in the Regulatory section.
By engaging stakeholders, your organization will get guidance and feedback, elicit buy-in, and drive collaboration to ensure success. Below, is a list of stakeholders and stakeholder groups that should be identified and engaged before beginning the process of opening a PACE.
- State and federal agencies
- National Pace Association (NPA)
- Hospitals and Urgent Care Clinics
- Other PACE organizations
- Specialty providers
- Consultants and Technical Assistance Centers (TACs)
State and Federal Government Contacts
The PACE application process involves extensive requirements at the state and federal levels. Develop contacts at both the state and federal levels. Although these relationships will grow and develop over time, it is wise to contact state and federal regulatory offices to get to know these stakeholders early in the process of starting a PACE organization. These stakeholders will be able to identify relevant regulations and regulatory processes, however, they may not be able to provide interpretation of regulations: consultants are more effective for regulatory interpretation. Specifically, build relationships with the CMS regional or central office staff and the Medicaid agency staff.
National PACE Association (NPA)
The National PACE Association (NPA) contains a wealth of information for new and existing PACE organizations. In addition to providing free resources for those looking to start a PACE, NPA offers a multi-tiered membership program. Membership options include: “Exploring PACE Membership,” “Prospective Provider Membership,” “Provider Membership,” and “Capitated Provider Membership.” For those in the category of exploring PACE or prospective providers, the NPA memberships offer a range of services from technical assistance and strategic planning to federal policy support and peer-to-peer learning.
Hospitals and Urgent Care Clinics
Identify nearby urgent care clinics and emergency departments and build relationships with administrators and providers who work there. Getting participants comfortable using urgent care centers rather than defaulting to the emergency department will save money. Additionally, having strong relationships with both urgent care clinics and emergency departments raises the likelihood that PACE will be notified when one of its participants shows up for unscheduled care.
Other PACE Organizations
In addition to NPA, several states also have PACE associations, which can help make connections with other local PACE organizations that have already gone through the startup process. Other PACE organizations, whether in the same state or elsewhere, can serve as invaluable resources from which to learn. See here for a list of states with PACE organizations.
Consultants / Technical Assistance Centers (TACs)
Consultants or PACE TACs can be instrumental in supporting the process of opening a PACE site and can provide expertise and support. Before hiring a consultant, identify the topic areas where support is needed to ensure that the assistance received is targeted and spending is efficient. Examples include
- Organizational and market assessment (see Organizational and Market Assessment section)
- PACE application preparation
- PACE facility development
- Staff hiring and training
- Program policy and procedure development
- Marketing and census building
- Quality improvement planning and implementation
- Financial reporting and monitoring
- Data collection and training
The National PACE Association (NPA) provides a list of TACs that can provide support. Additionally, since many existing PACE organizations have hired consultants, reaching out to other PACE organizations directly to identify potential consultants or consulting groups may be an effective strategy.
Other Stakeholders
Other entities in the community may have a vested interest in the PACE population or the development of a PACE organization. Make a list of community stakeholders and conduct outreach to create relationships early on. Examples of other stakeholders include health providers, housing centers, community coalitions, Area Agencies on Aging, and others who may refer participants to PACE. These groups or individuals can likely provide helpful feedback and guidance about the community. Additionally, community-based organizations, religious organizations, federal qualified health centers (FQHC) and other clinics, local service agencies, disease-specific groups, non-profits, and other long-standing community supports may interact with older adults regularly and be excited to partner in improving the coordination of health for their community.
Opening a PACE requires a considerable financial investment. There are significant initial expenses that occur before the PACE organization can even start serving participants, meaning they will need to be funded before receiving any payment from Medicare and Medicaid. These expenses may include several months of rent and staff salaries. One conservative estimate for an efficient start-up process is $5-6 million; however, it is generally recommended to have $8 million set aside to start a PACE.
To determine the total start-up funds needed and the source of start-up funding, work with the sponsoring organization and any funding partners to determine the financing terms. Banks and local foundations may provide funding or in-kind donations to support opening a new PACE. If attempting to secure new sources of funding, reach out to financial institutions that prioritize supporting community development. Some examples of such partners include Capital Impact Partners, Capital Link, National Cooperative Bank, Quantified Ventures, Social Innovation Ventures, and the John A. Hartford Foundation.
Financial Proforma Analysis
Complete a financial proforma, which should include a financial analysis and sensitivity analysis, as described below:
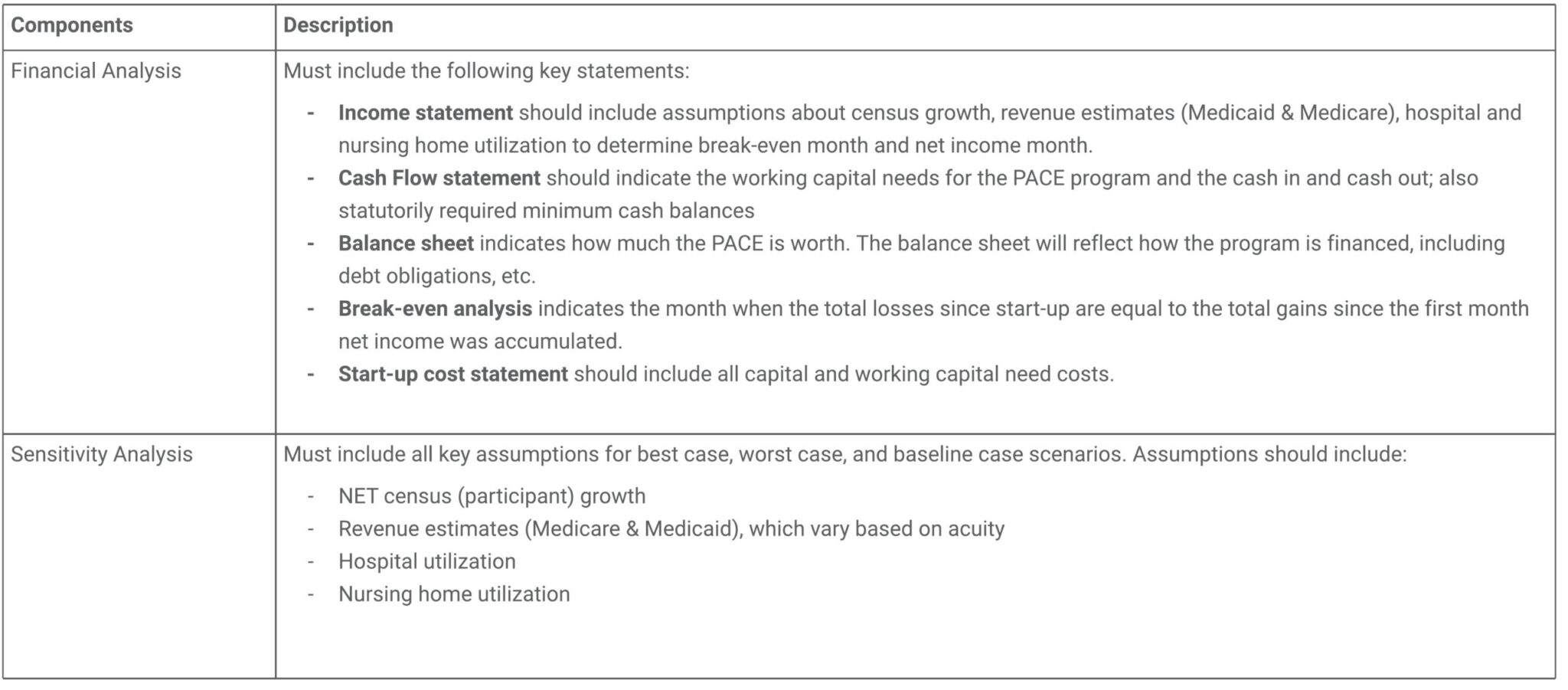
Consider using NPA’s High-Level PACE Financial Proforma as a guide or template when completing this step.
Accounting and Financial Reporting
When setting up accounting processes, be sure to consider all internal and external financial reporting that will need to be done. Review the state and federal financial reporting requirements prior to setting up the chart of accounts. After developing a clear understanding of the reporting that is required at the state and federal levels, proactively set up the chart of accounts to mirror that reporting.
Diagnostic risk adjustment data must be reported to CMS. This includes participant information, such as provider visits, hospitalizations, and treatments. This data feeds into the PACE organization’s per member per month (PM/PM) calculation, since PACE will receive a higher rate for caring for more frail and medically complex participants, and a lower rate for caring for less frail, healthier participants. Review the CentraCare PACE presentation “Mitigate the Risk in Risk Adjustment: It Takes a Team” to learn more about risk adjustment.
Financial Projections
As part of the application process, new PACE organizations must show financial projections for 18 months prior to opening and for 3 to 5 years after opening. Take a conservative approach to these initial assumptions to help meet projections.
Be specific when assuming wage rates and do not use global averages. Wages for different positions vary greatly by location and choosing to project based on global averages may not be conservative enough based on the location of the new PACE.
Insolvency Plan
Federal requirements mandate that PACE organizations have a documented plan in the case of insolvency, which must be approved by CMS. The insolvency plan must cover continuation of benefits for the duration of the period for which capitation payment has been made; continuation of benefits to participants who are confined in a hospital on the date of insolvency until their discharge; and protection of participants from liability for payment of fees that are the legal obligation of the PACE organization. Some states may also have additional insolvency requirements. Ensure that an insolvency plan is in place and meets all federal and state guidelines.
Insolvency may occur when the PACE organization when the cost to care for its participants is much higher than its operating revenue. To reduce the risk of insolvency, many PACE organizations purchase reinsurance prior to opening. Reinsurance plans can be purchased by PACE organizations to provide coverage for expenses beyond the capitated payments. NPA has partnerships with Aon Risk Services and Presidio Excess Insurance Services to provide PACE organizations with reinsurance products. The NPA reinsurance program offers several advantages including risk that is spread across the entire participating PACE population but policies that are individualized by PACE organization with complete flexibility over program design. Research these products and purchase one prior to opening.
The regulatory process is one of the most cumbersome parts of opening a PACE. CMS has created a document for all new applicants and existing PACE organizations seeking to expand a service area, detailing the steps required to apply to open a PACE. The document goes into detail about the steps necessary to open a PACE, including submitting a Notice of Intent to Apply, applying for a particular service area, requirements for policies and procedures, and completing the readiness review. Read and follow these steps closely.
The PACE regulatory guide references The Electronic Code of Federal Regulations (e-CFR) for PACE throughout. Review this and ensure the new program abides by all federal regulations.
Before opening, PACE must pass readiness reviews by both CMS and the state. These are separate reviews, so coordinate with the specific state Department of Health or Medicaid Office to understand the process. Keep in mind that regulatory processes may vary considerably by state.
Review the CMS Readiness Review Tool for PACE to understand the requirements. Use a consultant to complete an internal dry run inspection as a method to address as many flagged issues as possible before the actual inspection.
Every PACE organization must develop, implement, maintain, and evaluate an effective, data-driven, collaborative, written quality improvement (QI) program. The PACE organization’s Quality Director should work closely with the Executive Director and Medical Director to create this QI plan. The measures in the QI plan must be regularly reported on and improvement strategies must be implemented. Outcomes should be based on current clinical practice guidelines and professional practice standard. Some outcome measures, such as influenza vaccination rates, must meet or exceed minimum levels of performance set by CMS and the State administering agency.
The QI program must also include outcomes related to:
- Utilization of PACE services, such as decreased inpatient hospitalizations and emergency room visits
- Caregiver and participant satisfaction
- Outcome measures that are derived from data collected during assessments, including data on physiological well-being, functional status, cognitive ability, social/behavioral functioning, and quality of life of participants.
- Effectiveness and safety of staff-provided and contracted services, including competency of clinical staff, promptness of service delivery, and achievement of treatment goals and measurable outcomes.
PACE quality data is due to CMS every quarter, with a deadline of 45 days after the last day of the quarter. Follow the PACE Quality Monitoring Integrated User Guide step-by-step guide on reporting PACE data to CMS quarterly. Review CMS’ PACE Quality Monitoring & Reporting Guidance and PACE Organization Monitoring and Auditing for more information about reporting, monitoring, and auditing.
State administering agencies (SAAs) organize funding and administration for many state processes and often require reporting. Since each state is different, reach out to the state’s SAA to identify the relevant requirements.
After conducting a market assessment and identifying a service area, a physical location for the PACE center must be chosen. Having an address for the new PACE center is required for parts of the CMS and state applications, as described in the Regulatory section, so finding a location must be done early in the process.
Identifying a Location
When considering a physical location for the PACE center, map out the zip codes that will be served by PACE and the areas within those zip codes where the largest concentration of PACE-eligible individuals reside. Next, look for a place that is central to the greatest number of PACE-eligible people. Having a central location will ease the burden of transporting participants from their homes to and from the PACE center and other off-site service locations. Also, if possible, find a location for the PACE center that is as close as possible to hospitals, urgent care centers, public transportation, major roadways, and housing for underserved seniors. To support this effort, overlay a map of the geographic area of focus with public transportation routes, major roadways, housing for underserved seniors, specialty care providers, and hospitals and urgent care centers. Once the map is created, identify available spaces that are centrally located. Do research and visit these neighborhoods to ensure that they are safe from crime, dangerous traffic patterns, poor lighting, and challenges posed by inclement weather that could be avoided or rectified at a different location.
Locating a PACE Center Facility
Once a general location is chosen, next look for a building for the PACE center facility. When choosing a PACE center facility, it is important to have foresight about plans for the PACE organization. For example, decide on a target participant capacity to choose a space that can accommodate a full program – including enough staff to support a fully operational program. Additionally, make a list of priorities for the space and refer to these priorities when trying to decide on a space. Some example considerations:
- Day center space with windows and natural lighting
- Availability and size of outdoor space
- Ample parking lot space that accommodates PACE employee parking and PACE van pick-up and drop-off needs
- Accessible interior layout
- Dedicated quiet and private areas
- Dedicated space for physical and occupational therapy
- Kitchen space
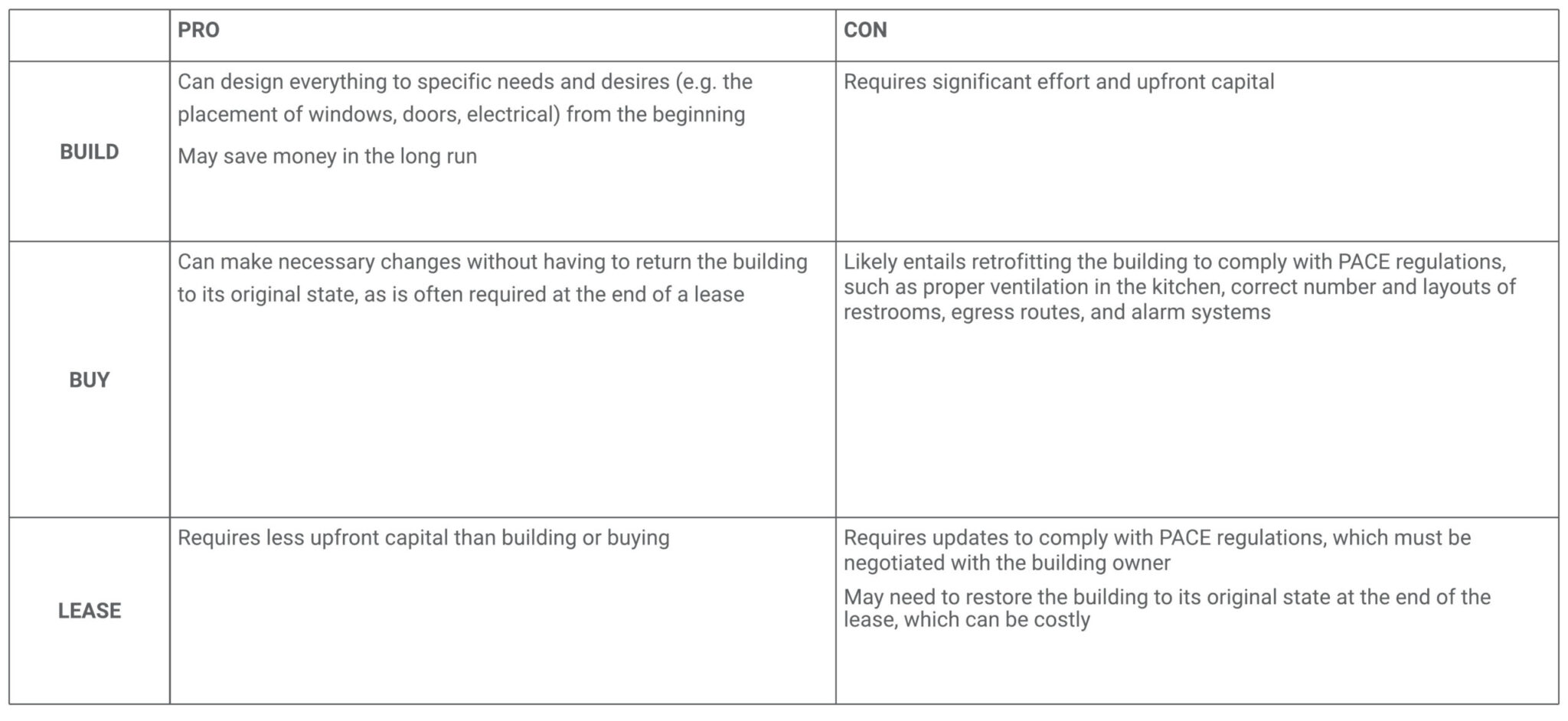
Preparing and designing the PACE center is a key piece of the process of opening a PACE facility, as this will be the hub of all PACE activities. Refer to the Principles of Effective Design, Layout and Furnishing of PACE Day Centers report for information about how to design a PACE center. This report is the outcome of a study conducted at the University of North Carolina and includes perspectives from 100 staff members of 13 PACE sites on the design of their centers. Use the information in this report as a resource while in the preparation and design phases.
Building Preparation
Building preparation is an important part of the process of opening a PACE. The state readiness review includes an in-depth walkthrough of the premises to ensure that the facility is sufficiently prepared to open in that it meets requirements for the kitchen, clinic, and day center, amongst others. Therefore, it is advised to reach out to the SAA and request an interview with the individual who will complete the walk through to ask for the must-have state and OSHA requirements for the building early on. Also ask this person for a list of common mistakes to avoid.If leasing a building, be sure to have an attorney review the lease thoroughly for restrictions that would impede the work, such as an inability to modify spaces and structures to fit the needs of the organization or a requirement to return the space to its original state at the end of the lease, which could be cost prohibitive.If buying or leasing a building, be sure to a hire a well-respected contractor. Look for a contractor who has experience working with medical buildings (such as nursing homes), if possible.If renovating a building (either buying or leasing), be sure to meet with city officials to learn about their building approval processes. Plan to have the PACE sponsoring organization representative, an architect, a representative with a medical background, and city officials in attendance during this meeting. Discuss what the details of the plan that has been created and ask the following questions:
- What permits are needed?
- What are some barriers that may be encountered?
- Is there any noteworthy information about timing and best practices around building or modifying the building?
- What clinical accommodations need to be included?
If building or making changes to a building that is being purchased or leased, engage a building inspection firm with experience conducting inspections for commercial buildings. The firm should conduct inspections on (at least) the following building systems:
- Roofing
- Structural
- Electrical
- Heating, ventilation, and air conditioning (HVAC)
- Plumbing
- Grease inceptor tank
Indoor Space
As a first step, create a preliminary design sketch of a floor plan for the building, laying out space for offices, dining, health care, rehabilitation, etc. This can be done in-house or by an architect or a space planner. Ensure that the design meets the latest egress codes, which are critical for fire safety.When planning office space, plan for the space that will be needed once the center is at full capacity rather than what will be needed when the program first opens its doors. Failing to plan for the future can result in a lack of office space for staff or separated teams. Decide on the number of participants per full time employee (FTE) and use the target program capacity to determine the number of staff the building needs to accommodate in the future. There is more information about how to do this in the Staffing Ratios subsection within the Staffing and Onboarding section.Assign separate offices for staff who will need to have private conversations, such as the Executive Director, Medical Director and social workers, at minimum. Be sure to include additional private rooms that can be reserved and used by staff on an as needed basis. A common mistake is to have too few of these private rooms, which can cause problems when the program is at full capacity. These private rooms will need floor-to-ceiling walls and may need additional soundproofing measures to ensure privacy.The layouts of many PACE centers emphasize the main gathering space, which is the Day Center. In addition to this central room be sure to create separate spaces for participants to gather and socialize, such as a computer lab, art room, and a TV/movie area. This can include building physically separate rooms as well as utilizing room dividers and will be particularly important as your census grows to hosting multiple activities at once.Sensory rooms, also known as Snoezelen Rooms, are used to help people with dementia or other disabilities use their senses to stimulate and activate or relax and calm, as needed. Consider including a separate sensory room in the PACE center design plans. For a detailed guide on how to create a sensory room for participants with dementia, visit the Kingston University London page.Aside from the general floor plan, be sure to address the clinically necessary design features listed below.
- Design all spaces with tile, linoleum, or a similar hard smooth floor surface since floors must be cleaned and disinfected often.
- Ensure stretcher access throughout the center and particularly through main hallways that lead between the clinic area and the entrances/exits. One PACE center that did not consider this had to lift stretchers above their heads to get them over a corner to transport patients.
- Design the clinic to be wheelchair accessible, considering door width and bathroom size.
- Cut corners in participant hallways at 45-degree angles. Since a person in a wheelchair cannot look around a 90-degree corner until they are already in the intersection, making the corners 45 degrees will reduce the risk of injury to both participants and staff.
- If the building is more than one floor, ensure elevator access.
- Purchase furniture that is accessible to all individuals, including large chairs and other seating options.
Emergency Power
Since the PACE center will provide crucial functions, participant lives may depend on the power to the building and all systems within the building. Mitigate risks associated with power outages by setting up a generator. Decide whether the generator will use diesel fuel or natural gas. Diesel generators require regular servicing to keep the diesel fuel effective but are not likely to be interrupted by natural events, like earthquakes. Natural gas generators hook up to a building’s gas lines and are easier to install. They are more often used due to ease of installation and maintenance, though they run the same risk of interruption as any natural gas connection.Determine which systems or equipment should be on emergency power. There are cost savings associated with having targeted areas covered by emergency power instead of covering the entire building. Examples of systems or equipment that can be put on emergency power include:
- Fire safety sprinkler system
- Exit lights (many lighting systems have backup batteries built in)
- Electrically operated doors
- Heating and cooling systems
- Oxygenation machines, laboratory and medication refrigerators, telephones/communication
Parking
The PACE center parking lot must have ample parking spaces for participants, visitors, and staff. Use the target program capacity and related number of staff to estimate how many parking spots are needed. Consider creating assigned parking spots for personnel, participants, and/or buses, especially if sharing a parking lot with other buildings. Some PACE centers separate employee parking from participant parking.The Americans with Disabilities Act (ADA) provides guidelines for what constitutes accessible parking, how many accessible parking spaces are needed, modifications for medical facilities, signage, maintenance, and other relevant topics. Review these guidelines and ensure that the parking lot design complies with ADA regulations.Be sure to include a separate space for PACE transportation vehicles to load and unload participants. Use the target program capacity to estimate the total number of vans needed at full capacity (many PACE centers have well over a dozen vans operating at any one time). Since most PACE participants will arrive and depart at roughly the same times each day, backups can occur. Create a designated area in the parking lot, free from other traffic, that PACE vans can load and unload. Although van bays take up a significant amount of space, they are a good option to allow participants to board and depart vans without rushing or requiring participants to walk across the lot or in front of vehicles when entering or departing from vans. Additionally, ensure that there is enough parking for the vans when they are not in use.
Hiring and training staff is a critical part of the process of starting a PACE. This section provides information about participant to staff ratios, the hiring process, specific roles that will need to be hired for, and onboarding.
Before beginning the hiring and onboarding process, review the CMS regulations for PACE Organization’s Relationship with Health Care Providers. This document provides important regulations that must be followed when staffing a PACE organization, such as required credentials for clinical staff.
Staffing Ratios
Determining an appropriate staff-to-participant ratio is an important first step in setting up comprehensive staffing. The staffing ratio will depend on the types of clinic staff that will be hired to run the program. For instance, a plan to have medical doctors (MDs) and no nurse practitioners (NPs) will result in a lower ratio of participants per one MD vs. a clinic with MDs and nurse practitioners. These decisions are typically dependent on the budget, so it’s critical to understand the average cost for each role.NPA’s Financial Benchmark Reporting is a member service that allows participating organizations to view PACE staffing data reports. Use this tool to help determine staff to participant ratios based on the type of clinical staff roles hired. Data from a 2015 PACE staffing survey, may also be helpful and can be found here.Plan for future staffing needs by building in buffers for the time it takes to hire and train new individuals based on the growing participant census. For instance, if working with a social worker ratio of one staff per 50 participants, plan to hire a second social worker as the participant census approaches 100. For example, begin the hiring process as the census reaches 75 participants to ensure adequate time to hire and onboard new staff without causing burnout of existing staff.
Hiring and Staff Positions
Many PACE organizations find it easier to hire some services through contractors, particularly when new or in the trial period. Once a participant population is more established, the decision to provide some services via PACE staff members versus via contractors may change. Fill out the Internal vs. Outsourced Hiring Worksheet to determine which PACE services will be delivered by staff versus external contractors. The worksheet supports comments, budgeted per member per month (PMPM) capitation rates, and candidates under consideration. The worksheet can be adapted to fit individual needs. See more information on hiring vendors and contractors in the Vendors and Contractors section.As a starting point, hire a human resources (HR) position. HR positions are typically responsible for recruitment, hiring, performance management, development, and compensation, so it would be wise to bring a HR position on board as a first step.Create detailed and specific job descriptions for every open position. Be sure to indicate all the specific skills candidates would need, even if they seem obvious. Schedule check-ins with the HR department or hiring team to review job postings and progress.Review the NPA’s Sample PACE Job Descriptions for more in-depth descriptions of the positions that must be filled at PACE.Every PACE organization needs a management team. See below for the specific roles that should be included in the management team:
- Executive Director (ED)
- Chief Medical Officer (CMO) or Medical Director
- Chief Financial Officer (CFO) or Director of Finance
- Compliance Officer
- Accountant
- Sales & Marketing Manager
- Network Manager
- Member Services Manager
- Case Manager
Review the Core Resource Set for PACE (CRSP) Sample Organizational Chart to get an idea for how staff can be organized.
In addition to the management team, it is advised to hire legal counsel or have a lawyer on retainer, as well as hiring an individual dedicated to quality from the onset. The quality person will be responsible for overseeing policies and procedure and review processes. Review the Regulatory section for more information about quality.
Interdisciplinary Team
Beyond the management team, all members of the Interdisciplinary Team (IDT) must be hired. The IDT is a foundational, crucial piece of the PACE model and provides the integrated, personalized care each participant needs. Refer to section 1 of the CMS PACE manual for more information about the composition of the IDT.Members of the IDT may be hired as internal staff or contracted. It is important to understand the certification or licensure requirements for each position. These may vary by state but often include the Medical Director, nurses, and medical assistants. It can also include personal care attendants and home health aides as well as transportation, dietician, and rehabilitation services. Ensure that IDT candidates have the required authorizations prior to hiring them or make plans with candidates to complete authorizations before their date of hire.Look for several qualities, beyond education and experience, that will translate to success at a PACE center when hiring individuals to work at the PACE center. These qualities include:
- Passion and motivation for learning and can process a significant amount of information in a short time
- Entrepreneurial spirit, potentially evidenced by experience with a startup company or having run their own business, to support proactivity in spaces of ambiguity
- Innovative and creative thinking and problem-solving tendencies to develop a program from the ground up
- Interpersonal skills to foster relationships with participants, specialists, urgent care providers, hospitals, and more
- Strong team player mentality to support teamwork in the particularly flat hierarchy of the IDT
- Passion for working with older adults
- Person-centered mentality for helping participants define and achieve their personal goals
- Understanding of value-based care principles
- Prior PACE experience (nice to have, but not critical)
Onboarding
PACE organizations should make a commitment to invest in training and onboarding, as strong onboarding can increase staff satisfaction and reduce turnover. Onboarding and training are still important for new staff members who have previously worked with other PACE organizations, as the operations and culture may have been different.As a first step, create a training catalogue for all new hires with all trainings, the staff that need it, and the timeframe in which it should be completed. The training catalogue should be aligned with the program’s policies and procedures document. Crosswalk the training catalogue with the policies and procedures to ensure that all trainings are covered in the policies and procedures and all relevant policies and procedures are covered with a training.See below for some examples of training topics:
- Clinical Operations
- Clinical Best Practices
- Home Health Best Practices
- Infection Control
- Using the EMR
- HIPAA Compliance
- Day Center Operations
- Emergency Plan
- Restraints
- Managing Wandering
- PACE Management
- PACE 101
- Ethics Training
- Information Technology (IT) Onboarding
- Payroll and Benefits
- Human Resources (sexual harassment, fraud and abuse, etc.)
Use the training schedule to compete a Staff Onboarding Checklist for each new staff member. Make a separate list for what trainings contractors will need, as this may not be the same as the staff member list. Work with the staff member/contractor to complete their onboarding checklist within a reasonable timeframe. Keep each staff member’s onboarding checklist on file to ensure regulatory compliance.
Although there are PACE services that are not typically outsourced, like primary care, there are many that can be. The decision of whether to have programs insource or outsource depends largely upon volume of participants and need for services. Therefore, PACE organizations may change how they source a program as they enroll more participants and needs change. These decisions will be program-specific and should be made based upon available data.
Using Vendors and Contracts vs. Hiring Internally
See below for a list of pros and cons for using vendors and contractors as opposed to hiring internally.
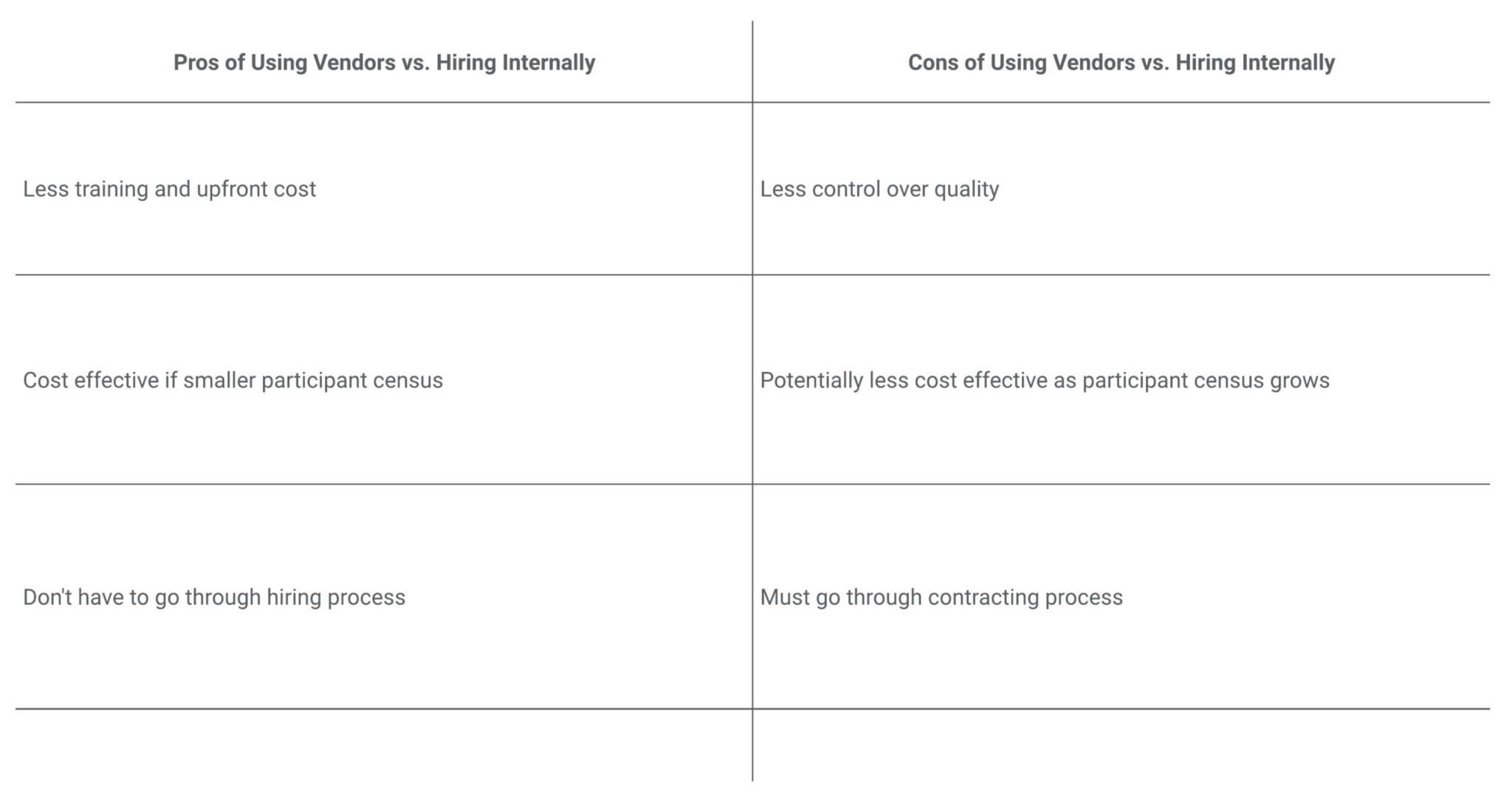
Before beginning the vendor and contractor contracting process, review the CMS regulations for PACE Organization’s Relationship with Health Care Providers. This document provides important regulations that must be followed when staffing a PACE organization with contracted staff and vendors. Ensure all regulations are carefully abided by.Use this worksheet to track decisions about insourcing vs. outsourcing certain services. Place an X in the Insource or Outsource columns based on whether planning to insource or outsource each PACE service/role, based on the budgeted PMPM rate, candidates being considered, and other comments.The NPA has created a Shared Services Program and all products and services offered through that program are evaluated in partnership with volunteer task forces comprised of PACE personnel. Once optimal options are identified, NPA negotiates with vendors to ensure affordable pricing and a high quality of services. The Shared Services Program provides NPA members with lower-cost products, PACE-tailored products and services, increased quality and efficiency, and assured continuity of function.” This program includes options in the following categories:
- Claims Processing with Encounter Data Reporting
- Home Technology Solutions
- Insurance and Reinsurance Products
- Participant Satisfaction Measurement
Specialty Providers and Provider Networks
Caring for PACE participants requires expertise beyond what is available among the IDT. Many PACE organizations find that their participants require significant dental, ophthalmology, podiatry, and mental/behavioral health specialty care. The primary areas that need to be addressed are:
- Physician Care
- Nursing
- Prescription Medications
- Dentistry
- Podiatry
- Optometry
- Audiology
- All Medical Specialty (cardiology, pulmonology, nephrology, oncology, ophthalmology etc.)
- Labs, X-ray
- Dialysis
It is wise to begin identifying and developing contractual relationships with local specialists to whom participants can be sent as early as possible. The National PACE Association website provides useful sample provider contracts.
PACE participants probably represent a small proportion of the patient population in the specialty provider network. Invest heavily in these relationships early to ensure that providers understand the PACE care model and goals and to ensure that participants can be seen on short notice.
Providers must meet several regulatory and reporting requirements to treat PACE participants. Assign a staff member with clinical experience to review provider networks to ensure that they meet all requirements to serve participants.
Once the program has operated for 6-12 months, perform an analysis of the use of specific specialists to determine whether the specialist program is operating as efficiently as possible and to assess the quality and timeliness of the care provided by the specialist partners. Additionally, assess which of the specialist visits could be conducted using telehealth and/or eConsults – both of which can reduce the amount of time it takes to get participants in to see specialists, reduce transportation costs and potentially reduce the cost of the care itself.
Process for Vendor or Contractor Selection and Contracting
Use this process that outlines each step from identifying vendors/contractors to approving them for service for each vendor or contractor under consideration.
Transportation Vendors
PACE organizations must provide their participants with transportation to and from the PACE clinic/day center and all medical appointments, which can be costly and logistically complex. A decision that must be made is whether to outsource or insource transportation services. Managing the timing of pick-ups and drop-offs, routes, drivers, and parking of many vans at once is complicated and may be most efficient if specialized software is purchased to optimize routes.If interested in outsourcing transportation, look for companies that have experience with PACE specifically, or with a senior population generally. Check with nearby nursing home facilities or other healthcare settings that serve seniors to get recommendations for reputable transportation services. If outsourcing transportation to drivers that do not have PACE experience or training, be sure to plan training for them.
Food Vendors
PACE organizations must decide whether to outsource day center meals or have an in-house kitchen and staff to prepare meals. It may make more sense to pay a third party to deliver meals to the day center when there is a low number of participants eating meals at the center. Outsourcing meals allows for less staff and lower cost to manage a kitchen and prepare food for only a small number of participants. In contrast, once the program grows and delivers a significant number of meals each day, it may make more financial sense to pay for extra staff to manage the kitchen and prepare the meals.PACE organizations must also be able to make specialized meals to meet the needs of their participants. Participants may need food that is low salt, Kosher, pureed, gluten free, or specialized in many other ways. The PACE organization should account for these needs when deciding whether to insource or outsource meals.
After-Hours Call Service
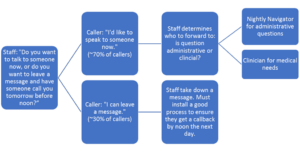
PACE organizations must decide whether to implement an insourced or outsourced after-hours call service. After-hours call lines staffed by nurses can help triage PACE participants when emergencies occur while the PACE clinic is closed.If implementing an outsourced after-hours call service, ensure that call staff have access to the participant medical records and provide all required training. If call staff have access to the participant’s medical record via the EMR they can ask very specific questions – “Did Ms. X get her meals delivered this week? How was Mr. Y’s colonoscopy yesterday?” – which can greatly improve the care provided and caller satisfaction. Staff can then add detailed documentation about the purpose of the call for the IDT to review the next day.
Home Health Services
Home health is another service that can be outsourced to a vendor. Home health vendors may have restrictions around their services, such as only being available in four-hour windows; take these restrictions into account when choosing whether to outsource or insource. Additionally home health is usually reimbursed through Medicare for a daily rate. As such, a more complex contract, with per diem or hourly rates, may be required if outsourcing.Regardless of the decision to outsource or not, PACE must be licensed to provide home health care. Ensure appropriate state home health licensure prior to the state readiness review.
Durable Medical Equipment Vendors
Durable Medical Equipment (DME) includes equipment and supplies ordered by a health care provider for everyday or extended use, such as oxygen equipment, wheelchairs and scooters, walkers and crutches, CPAP machines, or hospital beds. Contract with a vendor to acquire the equipment and manage its distribution and use. Do a significant amount of comparison between DME providers, as some providers may have delivery restrictions.
Nursing Homes, Skilled Nursing Facilities (SNFs)
There will be instances in which PACE participants need nursing home or SNF care. Find nearby nursing homes or SNFs and cultivate strong, working relationships with them. If the individuals in leadership there do not have experience with PACE, be explicit and upfront about the priorities for participant care. Some PACE organizations have had challenges with local nursing homes since a fee-for-service payment model incentivizes nursing homes to keep patients for the maximum of 21 days, regardless of patient need. Additionally, high turnover in nursing homes make ongoing education around the PACE model of care an enduring priority.
Third Party Administrators (TPAs)
Clinical providers that see PACE participants will submit their claims to a Third Party Administrator (TPA) for payment by the PACE organization. The TPA will compare the claim to the contract between the provider and PACE and will approve or denies the claim. The TPA also handles all reporting to CMS. TPA services typically charge a percentage fee based on the size of the participant population, so costs will increase as the participant populations grow.New PACE organizations must decide on a TPA to work with. Major TPA contractors include PeakTPA, and Tabula Rasa HealthCare.
Prepare to set up systems to collect and report many types of data from different data collection systems. This data will be used for reports submitted by vendors, to file Medicare and Medicaid claims, and complete quality improvement reports. Below are the systems needed to establish to support data collection and reporting.
Electronic Medical Records (EMR) Systems
EMR systems are essential to collection and aggregation of all patient data. Work with IT staff to understand how prospective EMR systems would need to fit within the organization’s IT framework. Select an EMR system that meets the following requirements:
- It must support the unique workflow of the practice. There are some idiosyncratic aspects of the PACE clinical model, such as the involvement of each member of the 11-member IDT, who must assess the participant periodically. Make sure the EMR can assimilate these assessments into an intelligible care plan.
- It must be relatively easy to use. Some EMR systems are easier than others when it comes to putting information into the system and retrieving it when needed in a useable format.
- It must have excellent analytics. PACE organizations have very demanding requirements for analytics to support their Quality Assessment and Performance Improvement (QAPI) process.
- It must address claims coding in a meaningful way. This is important because coding has a direct impact on revenue through the risk adjustment process. Coding is typically handled with a superbill that is a function of the Practice Management System and should be built into the functionality of EMR systems oriented for PACE.
- It must be interoperable with other systems, like the TPA or Part D vendor, who will be adjudicating claims.
- It must be easy for the clinician to access a basic profile of the patient remotely.
- It must be a Software as a Service (SAAS) solution as opposed to a traditional software license purchase. The latter requires the user to build the server, configure the software, and maintain the instance on its own network. In a SAAS environment, the user can access the robust functionality of a SAAS solution from a laptop or desktop without any special software, hardware, or network configurations.
- It must meet the hardware, software, network, and security standards of the technical organization. It should address the increasingly stringent requirements for handling PHI.
Additionally, consider that while it is convenient to use a system that is customized for PACE (such as PACELogic), it is an efficiency challenge to choose one that requires the use of more than one program.
Review Leading Age’s white paper, “Electronic Health Records for Long-Term and Post-Acute Care: A Primer on Planning and Vendor Selection” when selecting and implementing an EMR system.
Medication Management Platform
New PACE organizations must decide on a medication management system, which will be used to manage participant medications. This is of importance for the PACE eligible population because they often have multiple conditions requiring medication.
Review the 2018 NPA Conference Presentation “Medication Management in PACE” for what to consider when choosing a medication management platform.
Customer Relationship Management (CRM) System
A CRM system is needed to collect and store data that is not already being captured in the EMR. This system should track marketing outreach to potential enrollees, financial information, interactions with participant family members, contact information, and many other important data points. Choose a CRM system that provides analytic tools to measure trends in participant census, financials, and service delivery. Salesforce and Oracle are both popular CRM vendors.
CMS has very specific PACE marketing requirements. Review chapter 3 of the CMS PACE Manual for all information about marketing requirements, including details about application materials, prohibited marketing activities, and other key marketing topics.
Application Materials
Several marketing materials must be included in the PACE application submission. Be sure to create the following materials to accompany the application:
- Website (in-development is acceptable)
- Brochures about the PACE organization
- One-page plan for community outreach
- PACE Center Logo
Outreach
Outreach is an important step in the process of starting a PACE organization, as the success of the organization depends on the ability to recruit participants.
Conduct outreach to other providers or organizations to enroll participants, such as housing developments, government officials, senior citizens, retiring physicians, or fiduciaries. Some examples of successful marketing outreach tactics include:
- Networking events with area senior professional organizations
- Speaker forum to senior groups, senior centers, and religious groups using PACE 101 as topic
- Tours of day center
- Outreach to and one-on-one meetings with city mayors, council members, and county supervisors
- Outreach to and meetings with area US Department of Housing and Urban Development (HUD) management and local housing authorities
- Medical Director meetings with area medical professionals to increase comfort transitioning patients to PACE
- Other advertising tactics, such as radio ads, billboards, bus signs, etc.
To protect privacy, the state owns the addresses of individuals who qualify for PACE. Submit marketing materials to the state and the state will mail those materials to potential participants. This process can take many hours for coordination and may yield a relatively low number of participants, so it should not be the only option pursued.
Marketing Materials
Ensure all marketing materials are culturally and linguistically relevant and appropriate to the community the PACE will serve.
Create a one-page “leave-behind” document to distribute to providers or the general community to stimulate partnership and enrollment. The upper half of the document should include the full PACE name, the year it is opening, and a high-level summary. The lower half of the document should include a comprehensive list of services offered, a note that care is coordinated and tailored to the participant, a description of the sponsoring organization opening PACE, and community partners.
Create materials with consistent branding to conduct effective marketing. Use focus groups to ensure effectiveness of marketing materials. Use this checklist when creating materials.